BSc 2nd Year Microbiology Infection and Disease Notes Study Material
BSc 2nd Year Microbiology Infection and Disease Notes Study Material: BSc is a three-year program in most of universities. Some of the universities also offer BSc Honours. Out of those, there are BSc 2nd Year Infection and Disease Notes Study Material, BSc Sample Model Practice Mock Question Answer Papers & BSc Previous Year Papers. At gurujistudy.com you can easily get all these study materials and notes for free. Here in this post, we are happy to provide you with BSc 2nd Year Microbiology Infection and Disease Notes Study Material.

BSc 2nd Year Microbiology Infection and Disease Notes Study Material
Host-parasite relationship
The word infection (derived from Latin) means to mix with or corrupt. The term refers to the relationship between the host and the parasite, and the competition for supremacy that takes place between them. If the host has the upper hand, due to increased host resistance it remains healthy and the parasite is either driven away or assumes a benign relationship with the host.
On the contrary, if the host loses the competition (may be due to increased pathogenicity), the disease develops. Thus diseases are the outcome of competition between the host and parasite. The disease is generally considered as any change from the general state of good health. But this does not present the true scientific nature of the disease, since the general state of good health may also be changed by a factor, other than a parasite. Thus the disease is a malfunctioning process caused due to continuous irritation by the parasite. Disease should not be confused with infection: a person may be infected without becoming diseased.
Normal flora
The concept of infection in the host-parasite relationship is expressed in the body’s normal flora. Normal flora is a population of microorganisms that infect the body without causing disease. Some organisms establish a permanent relationship, as E. coli is always found in the large intestines of humans. Others, like streptococci, are transient.
Symbiotic associations between the body and its normal flora exist at different levels. These may be in the form of mutualism or commensalism. Lactobacillus spp. in the human vaginas is an example of mutualism. They derive nutrition from the vaginal environment and the acid produced by them prevents the overgrowth of other microbes.
E. coli exists as a commensal, though may also sometimes exist in the mutualistic association. Normal flora exists on the skin, oral cavity, upper respiratory tract, latter part of the small intestine, and large intestine. In intestines, there are Bacteroides, Clostridium (spores), Streptococci, and Gram-positive rods including Enterobacter, Klebsiella, Proteus and Pseudomonas, E. coli Candida albicans. Normal flora undergoes changes in response to the internal environment of the body.
Pathogenicity
This term refers to the ability of a parasite to gain entry into the host’s tissues and bring about a change (anatomical or physiological) resulting in a change of health and thus disease. The word is derived from pathos (Greek) meaning suffering. The term pathogen has the same root and refers to an organism able to cause disease i.e. possessing pathogenicity. The symbiotic relationship between host and parasite is called parasitism. Parasites vary in their pathogenicity.
Even in the same taxonomic species, there may be non-pathogenic, less pathogenic, or many pathogenic strains. Some parasites of cholera, typhoid fever, and plague are known to cause serious human diseases, whereas others like common cold viruses are less pathogenic. (BSc 2nd Year Microbiology Infection and Disease Notes Study Material)
There are also opportunistic which exist as commensals in the body till normal defense mechanisms are suppressed when they invade the tissue and act as pathogens. For instance, Streptococcus pneumoniae lives on the surface of the upper respiratory tract. Pneumocystis carinii, Toxoplasma gondii, and Cryptosporidium spp. which are opportunistic otherwise, begin to invade the patients suffering from AIDS. Thus a shift in the body’s delicate balance of controls may convert infection to disease. Several factors may alter the balance of microbes. Destruction of normal flora by indiscriminate use of antibiotics may lead to diseases.
A new concept has thus emerged in recent years. Traditionally, microbiologists believed that organisms were either pathogenic or nonpathogenic. This distinction has been blurred by the fact that normally benign organisms may be pathogenic when body defenses weaken or fail. AIDS illustrates this concept very well. It is now recognized that pathogenicity is a function of the aggressive nature of the parasite as well as the level of resistance in the host. (BSc 2nd Year Microbiology Infection and Disease Notes Study Material)
Whereas pathogenic is used in a qualitative sense, virulence is used in a quantitative sense giving a measure of the extent of pathogenicity of a microorganism.
The term virulence is often used to express the degree of pathogenicity of a parasite. The term is derived from the Latin virulent, meaning full of poison. An organism such as the typhoid bacillus that invariably causes the disease is said to be highly virulent, whereas Candida albicans which causes sometimes the disease is called moderately virulent. Certain organisms, described as avirulent are not generally regarded as disease agents for example the lactobacilli and streptococci found in curd, etc.
However, it should be noted that any microbe has the ability to change genetically and become virulent. E. coli, for example, was long considered a virulent commensal of humans, but certain toxin-producing strains have been isolated that cause diarrhea and urinary tract diseases in humans. (BSc 2nd Year Microbiology Infection and Disease Notes Study Material)
The virulence depends in large part on two properties of a microbe: invasiveness and toxigenicity, important in human diseases. Invasiveness refers to the ability of a microbe to invade human cells and tissues and to multiply on or within them. Toxigenicity refers to the ability of a microbe to produce biochemicals, known as toxins that disrupt the normal functions of cells or are generally destructive to human cells and tissues. (BSc 2nd Year Microbiology Infection and Disease Notes Study Material)
Progress of disease
The disease is a dynamic series of events expressing the competition between the host and parasite. Most diseases follow a definite recognizable pattern of development. (BSc 2nd Year Microbiology Infection and Disease Notes Study Material)

The various phases of disease development that appear in sequence are as follows:
1. Incubation period. This is the initial phase representing the time between the entrance of the parasite and the appearance of symptoms. This is short of 1-3 days as in cholera, a moderate of two weeks as in chickenpox long as 3-6 years as in leprosy.
2. Period of prodromal symptoms. This phase is characterized by general symptoms such as nausea, fever, headache, etc. which indicate that the competition for supremacy has begun. (BSc 2nd Year Microbiology Infection and Disease Notes Study Material)
3. Period of acme. This is the acute phase when specific symptoms appear. There may be body rash, brain lesions, jaundice, skin ulcers, swollen glands, etc. There may be high fever and chills. (Infection and Disease Notes Study Material)
4. Period of decline or defervescence. This is the stage during which the symptoms subside. It is finally followed by,
5. Period of convalescence. During this time the body’s systems return to normal.
Transmission of Disease
The causal agents of the disease may be transmitted by a variety of methods. Broadly, all such methods could be divided into (i) direct methods and (ii) indirect methods.
[I] Direct methods
Such methods imply close or personal contact with one who has the disease. Kissing, hand-shaking, sexual intercourse, or contact with faces are examples. Diseases like gonorrhea and genital herpes and many diseases of the intestine are spread by direct contact.
Direct contact may also mean exposure to droplets, the tiny particles of mucus expelled from the respiratory tract during a cough or sneeze. Diseases spread by this method include influenza, measles, pertussis (whooping cough), streptococcal sore throat, etc. For some diseases such as rabies, leptospirosis and toxoplasmosis direct contact with animals is necessary.
[II] Indirect methods
These include consumption of contaminated food or water as well as contact with fomites. Foods may become contaminated during processing or handling or they may come from diseased animals. Poultry products are a common source of salmonellosis (Salmonella infects chickens). Pork may spread trichinosis (parasites that live in the muscles of pigs).
Fomites are inanimate objects (clothing, utensils) that carry disease agents. Bed linens may be contaminated with pinworm eggs. The contaminated syringe may carry hepatitis B viruses.
Arthropods are important means of indirect transmission. Living organisms that carry disease agents from one host to another are called vectors. Arthropods may serve as a mechanical vector if they carry agents of disease on legs and other body parts. The animal may serve as a biological vector. In malaria, yellow fever, etc. the disease organisms infect the arthropod and accumulate these in salivary glands from which they are injected during the next bite. In Rocky Mountain spotted fever and Lyme disease, microbes gather in the tick’s gut and enter a wound when the tick feeds on human skin. (BSc 2nd Year Microbiology Infection and Disease Notes Study Material)
There are some reservoirs of some diseases. These reservoirs serve as continuing sources of disease agents and are important in perpetuating the disease. In smallpox, the sole reservoir of viruses is humans. Meningococcal meningitis and diphtheria also have humans as reservoirs. A carrier is a special type of reservoir. Generally, a carrier is one that has recovered from the disease but continues to shed the disease agents. Thus persons who have recovered from typhoid fever or amoebiasis are usually carriers for many weeks after the disappearance of the disease symptoms. Their feces may spread the disease through contaminated food or water.
Animals may also be reservoirs of disease. Domestic housecats without showing symptoms may transmit toxoplasmosis, caused by Toxoplasma gondii to humans. (BSc 2nd Year Microbiology Infection and Disease Notes Study Material)
Types of Diseases
There are many terms to describe different types of diseases. Diseases are given different names on the mode of their transmission, geographic area of distribution, extent of severity, etc. The following terms are most common:
1. Communicable diseases. The diseases that are transmissible among hosts. These may be transmitted by direct as well as indirect methods. Some communicable diseases are further described as contagious since they pass with particular ease among hosts. Chickenpox, measles, genital herpes, etc. are contagious. (BSc 2nd Year Microbiology Infection and Disease Notes Study Material)
2. Noncommunicable diseases. These are singular events where the causal agent is directly acquired from the environment and is not easily transmitted to the next host. For instance, tetanus.(Infection and Disease Notes Study Material)
3. Endemic diseases. The disease usually occurs at a low level in a certain geographic area, such as toxoplasmosis.
4. Epidemic diseases. The diseases which break out in explosive proportions within a population, such as influenza, and measles.
5. Pandemic diseases. When an outbreak above the normal level occurs on a worldwide scale, as the influenza pandemic in many countries of the world.
6. Other types of diseases. For relative measurements of their severity, the diseases are described as acute and chronic. An acute disease develops rapidly, shows substantial symptoms, reaches a climax, and then fades out. Cholera, typhus, and yellow fever are examples. Chronic diseases tend to linger for long periods of time; symptoms development is slower, the climax is rarely reached and convalescence may continue for several months. Infectious hepatitis, trichomoniasis, etc. belong to this category.
Some acute diseases may turn to chronic if the body is unable to get rid of the parasite completely. Examples are giardiasis and amoebiasis. The individual in such cases may become a chronic carrier of the parasite and source of infection to others. One who harbors the parasite with no sign of the disease is called a reservoir. (BSc 2nd Year Microbiology Infection and Disease Notes Study Material)
A primary disease occurs in an apparently healthy body, whereas a secondary disease is in a weakened individual. In many viral infections, secondary diseases due to bacteria are common to develop, unless proper care is taken. Local disease is restricted to a single area of the body, such as the skin, whereas systemic diseases are those which have involved deeper organs and systems.
A staphylococcal skin boil begins as a localized skin lesion but may become serious when the organisms spread, causing systemic diseases of bones, meninges, or heart muscle. Bacteremia is the dissemination of bacteria through the bloodstream. Septicemia, an infection spreading in the blood is often used in the same sense. Fungemia refers to the spread of fungi; viremia to viruses and parasitemia to protozoa and multicellular worms, in the bloodstream.
Most diseases are caused by infectious agents and are known infectious diseases. However, there are also which are due to malfunction of a body organ or system. These diseases are called physiological diseases. There are also nutritional diseases such as beri-beri which are due to dietary insufficiency, and there are genetic diseases such as sickle cell anemia and phenylketonuria (PKU) that are traced to mutations in genes. (BSc 2nd Year Microbiology Infection and Disease Notes Study Material)
Establishment of Disease
The disease is the result of a complex series of interactions involving both the host and parasite. A parasite must possess some unusual potential characteristics which allow it to overcome host defenses and bring about the anatomical or physiological changes leading to disease. Before it can manifest these abilities, however, the parasites first gain entry to the host in enough numbers to establish a population. Then it should be able to penetrate and grow at that location.
The establishment of a microbially caused disease is infact a function (f) of the virulence of the particular pathogen in terms of its invasiveness, its toxigenicity, the dosage (numbers) of that pathogenic microbe, and the resistance of the host. It may therefore be expressed as follows:
Infectious disease X host resistance = f(microbial virulence X dose)
The relationship between a pathogen and its host is dynamic and varies depending on the microbe and the physiological state of the host and pathogen. We shall consider such factors that determine whether the disease can occur with a focus on the parasite.
1. Portal of entry. The avenue or portal of entry refers to the site at which the parasite enters the host. It varies for different parasites. These are wound for tetanus, intestines for dysentry bacilli, and lung tissue for pneumococci. Some have multiple portals of entry as the tubercle bacillus, which may enter by respiratory droplets, contaminated food or milk, or skin wounds.
2. Inoculum dose. It refers to the number of parasites that must be taken into the body in order for a disease to be established. For example, the injection of one billion typhoid bacilli in contaminated water will perhaps lead to disease. Cholera bacilli number may be even more, as most of them are susceptible to stomach acid.
3. Tissue penetration. Most information on this aspect is based on studies on histological preparations, tissue cultures, and animals. Understanding the penetration process of tissues is not complete. Once penetration has occurred, the parasites compete with the host cells for nutrients and minerals. The ability of a parasite to penetrate tissues and cause structural damage is invasiveness.
4. Enzymes. The virulence of a parasite refers to its degree of pathogenicity. Thus an organism may exhibit high, moderate, or low virulence.
Virulence is partly dependent upon the parasites’ ability to produce a series of enzymes directed at host defenses. These enzymes or factors contribute to the disease process by helping the parasite overcome host resistance, affecting tissue cells, and by interfering with physiological or biochemical processes in the host. In microbiology, such factors are also called aggressions.
5. Toxins. They are microbial poisons that have a direct effect on the tissues, organs, and physiological processes of the host, rather than on its defense mechanisms. Toxins are produced during the growth of the parasite and have a pronounced effect on disease development.
They cause discernible damage to human systems and in some cases even death. In the past, toxins produced by microbes were classified as exotoxins if they were heat-labile proteins secreted by the cell and as endotoxins if they comprised a heat-stable part of the microbial cell. However, we now know that some exotoxins are not released until the cell is disrupted and that substances classified as endotoxins are sometimes released from the cell without lysis. Therefore, a better classification system for toxins is one based on the biochemical nature of the toxin, whereby exotoxins are equated with protein toxins and endotoxins with lipo poly. saccharide (LPS) toxins.
[I] Protein toxins (Exotoxins)
In contrast to LPS toxins, the effects of protein toxins are specific to the microbe producing the toxin, and these toxins cause distinct clinical symptoms. Whereas LPS toxins are produced exclusively by Gram-negative bacteria, protein toxins are produced by both Gram-negative and Gram-positive bacteria. Most of these toxins are composed of a receptor protein component that attaches to a target cell and a toxic component that enters the cell and disrupts normal cell activity. They are more readily inactivated by heat than LPS toxins.
They can be normally inactivated by exposure to boiling water for 30 minutes, whereas LPS toxins can withstand autoclaving. Some enterotoxins, however, are peptides that relatively heat stable. (Microbiology Infection and Disease Notes)
Typically, protein toxins are excreted into the surrounding medium. For instance, Clostridium botulinum, causing botulism, secretes a potent protein toxin in canned foods. Protein toxins are generally more potent than LPS toxins, and far smaller amounts are needed to produce serious symptoms. For instance, about 30g of diphtheria toxin (a protein toxin) can kill 10 million people and 1g of botulinum toxin can kill over 225 million people. Protein toxins are named on the basis of the disease they produce or according to the symptoms they cause.
Thus neurotoxins affect the nervous system, enterotoxins cause inflammation of gastrointestinal tract tissues, and cytotoxins interfere with cellular functions. (BSc 2nd Year Microbiology Infection and Disease Notes Study Material)
1. Neurotoxins. They interfere with the functioning of the nervous system, usually by blocking nerve cell transmission. Neurotoxins, even those produced by members of the same genus, differ markedly in their mode of action. Neurotoxins responsible for botulism, caused by Clostridium botulinum, bind to nerve synapses, blocking the release of acetylcholine from nerve cells of the central nervous system and causing the loss of motor function. The inability to transmit impulses through motor neurons can cause respiratory failure, resulting in death. (BSc 2nd Year Microbiology Infection and Disease Notes Study Material)
The neurotoxin tetanospasmin, produced by Clostridium tetani, causing tetanus, interferes with the peripheral nerves of the spinal cord. The toxin inhibits the ability of these nerve cells to transmit signals to the muscle cells properly, causing spastic paralysis. As done by the neurotoxin of botulism this toxin also paralyzes the motor neurons. (Infection and Disease Notes Study Material)
The neurotoxin of Shigella dysenteriae, (Shiga toxin), interferes with the circulatory vessels supplying blood to the central nervous system rather than affecting nerve cells directly. (BSc 2nd Year Microbiology Infection and Disease Notes Study Material)
2. Enterotoxins. They stimulate the cells of the gastrointestinal tract. Various enteropathogenic bacteria like Salmonella, Shigella, and Vibrio spp. produce enterotoxins. The enterotoxin choleragen of Vibrio cholerae inhibits the conversion of cyclic AMP to ATP by increasing the activity of adenyl cyclase. (BSc 2nd Year Microbiology Infection and Disease Notes Study Material)
3. Cytotoxins. They kill cells by enzymatic attack or by blocking essential cell metabolism. They include the proteins that cause the lysis of blood cells and those which interfere with protein synthesis. For example, the diphtheria toxin of Corynebacterium diphtheriae inhibits protein synthesis in mammalian cells. It affects cardiac and renal tissues. This toxin blocks transferase reactions during the translation of mRNA. This is interesting to know that only phage-infected cells (lysogenised cells) of the bacterium produce toxins (the phage converts nonpathogenic cells to pathogenic). The protein toxin is coded for by the phage genome.
[II] Lipopolysaccharide toxins (Endotoxins)
The name given to these toxins is equated with the LPS component of the Gram-negative eubacterial cell wall. Although all Gram-negative eubacteria have LPS in their cell walls, LPS is not toxic unless it is released from the outer layer of the cell. When these bacteria die, their cell walls disintegrate and release the toxin. Some Gram-negative bacteria produce LPS while growing and their LPS may have a toxic effect on the host. Toxicity is associated with the lipid portion of the LPS molecule, termed lipid A (composed of fatty acids, such as B-hydroxy myristic). This same structure is found in all eubacterial Gram-negative LPS.
The physiological effects of LPS toxins include fever, circulatory changes, and other general symptoms like weakness and nonlocalized aches. The effects of LPS toxins are generally the same for all species of Gram-negative bacteria because of the common nature of lipid A. Thus there are no specific characteristic symptoms associated with the endotoxin of a particular species of bacterium. Species Of Salmonella and Shigella, besides LPS toxins, also produce protein toxins (exotoxins) and these are exotoxins that are largely responsible for their pathogenicity. Shigella produces a protein (neurotoxins).
The Human Circulatory System
The circulatory system of humans occupies a central place in disease development processes. This system serves as the principal vehicle for the dissemination of parasites and their toxins. It is also the circulation within which many important factors in the host defense system operate. These two aspects add to the importance of a basic understanding of the circulatory system and its capabilities. An outline of this system should also serve as a bridge between the disease process discussed in this chapter and the resistance process to be considered in the next. The emphasis will be on the blood and its components.
Blood components
There are three major components of the blood: (i) the fluid, (ii) the clotting agents, and (iii) the cells. The fluid portion, called serum, is an aqueous solution of minerals, salts, proteins, and other organic substances. When clotting agents such as fibrinogen and prothrombin are present, the fluid is referred to as plasma. The pH of arterial blood is about 7.35 to 7.45.
Three types of cells circulate in the blood: (i) the red blood cells or erythrocytes; (ii) the white blood cells, or leukocytes: and (iii) the platelets or thrombocytes. The erythrocytes arise in the bone marrow and carry oxygen to the tissues loosely bound to the red pigment hemoglobin.
A normal adult has about 5 million erythrocytes per cubic millimeter (mm) of blood. After circulating for about 120 days, the erythrocytes disintegrate in the spleen, liver, and bone marrow. The hemoglobin is then converted to bilirubin, a pigment that gives bile a deep yellow colour. Normally bilirubin is carried to the liver for degradation in a protein-bound form. However, if the liver is damaged, or if too many erythrocytes disintegrate, excess, bilirubin may enter the bloodstream. This condition is called jaundice.
White blood cells or leukocytes have no pigment in their cytoplasm, and when unstained are gray-coloured. These are also produced in the bone marrow. Their numbers are about 5-9 thousand per mm3 of blood and have different life spans depending on the type of cell. Different types of leukocytes in the blood are shown in Figure.
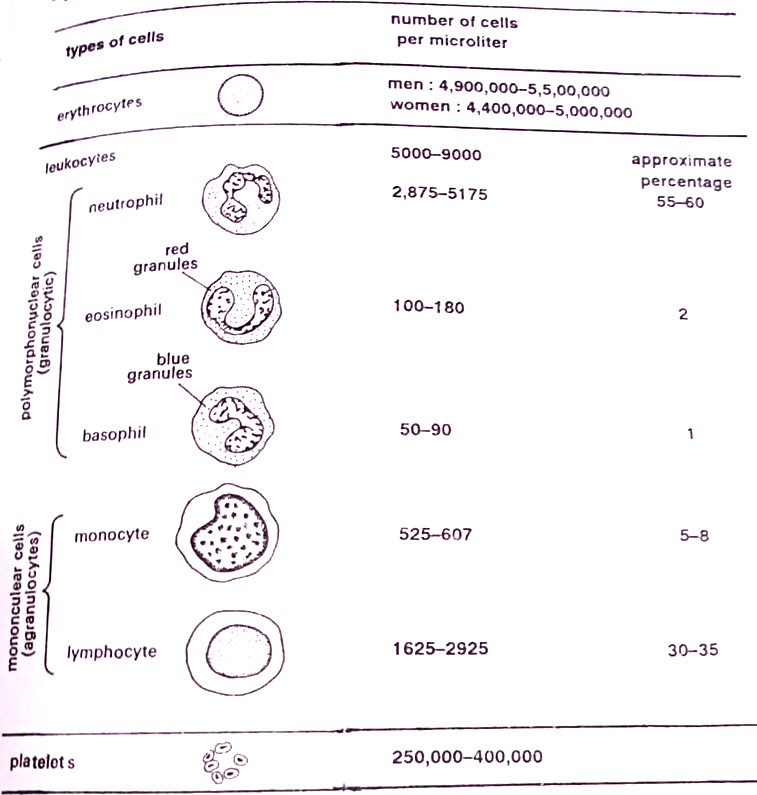
One type of leukocyte has a multilobed nucleus and is thus referred to as a polymorphonuclear cell or PMN. In its cytoplasm, it has many lysosomes that contain digestive enzymes. Depending upon how these granules stain, the cell is called a neutrophil, eosinophil, or basophil. The neutrophil stains with neutral dyes and functions chiefly as a phagocyte. They pass out of the circulation through pores in the vessels and squeeze into narrow passageways among the cells to engulf particles.
About 55 to 60 percent of the leukocytes are neutrophils. Basophils are those leukocytes whose granules stain with basic dyes. Their number is about 50 to 90 per mm of blood and represents about 1% of the total leukocytes. They function in allergic reactions, releasing histamine. Eosinophils are the third type of leukocytes, representing about two percent of the total number. They have red cytoplasmic granules with an acidic dye as eosin. They are said to neutralize the active chemicals in basophil granules.
Another major phagocyte of the circulatory system is the monocyte. This cell has a single, bean-shaped nucleus, occupying a major area of the cytoplasm. There are no granules. About 5-8% of the leukocytes are monocytes. They form a type of phagocyte called the macrophage. Another type of leukocyte is a lymphocyte. They are produced in the bone marrow and transported to lymph nodes. This cell has a single, large nucleus but no granules. Lymphocytes make up about 30 to 35% of the leukocytes in the human body and function in the immune system.
Blood platelets (thrombocytes), the third type of cells in the circulatory system are small bodies originating from cells in the bone marrow. They have no nucleus and function chiefly in the blood clotting mechanism.
Lymphatic system
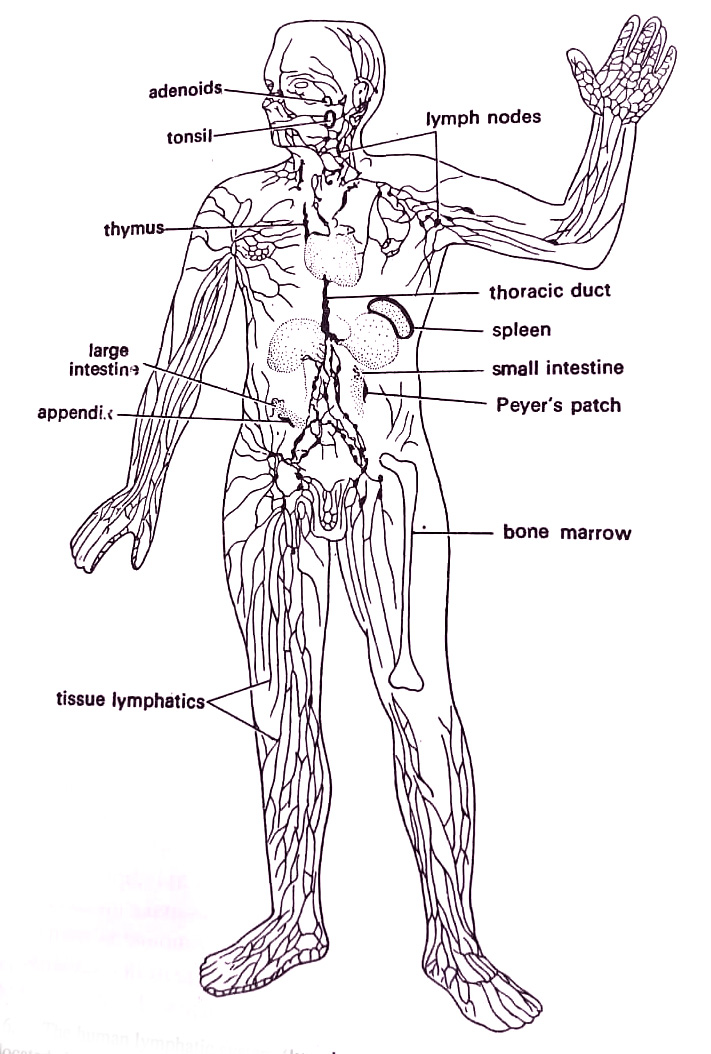
The fluid that surrounds the tissue cells and fills the intercellular spaces is called tissue fluid, or lymph. Lymph is similar to serum except that it has fewer proteins. Lymph bathes the body cells, supplying oxygen and nutrients while collecting wastes. It is pumped along in tiny vessels by the contractions of skeletal muscle cells. Eventually, the tiny lymph vessels unite to form large vessels that constitute a lymphatic system. The system empties into a large vein just before the heart. This system is thus interrelated with the circulatory system in man.
Pockets of lymphatic tissue located along the lymph vessels are known as lymph nodes. These are prevalent in the neck, armpits, and groin. They are reniform organs containing phagocytes that engulf particles in the lymph and lymphocytes and then respond specifically to substances in circulation. Lymph nodes become enlarged during disease time. The tonsils, adenoids, spleen, Peyer’s patches of the intestine, and appendix are specialized types of lymph nodes. (BSc 2nd Year Microbiology Infection and Disease Notes Study Material)
BSc 2nd Year Microbiology Infection and Disease Notes Study Material
BSc 2nd Year Sample Model Practice Mock Test Question Answer Papers